Understanding Leukemia: Symptoms, Diagnosis, and Treatment Options
Imagine someone who always felt healthy, only to suddenly start feeling unusually tired, getting frequent infections, or noticing unexplained bruises. These could be early signs of leukemia, but how many of us would connect those symptoms to cancer?
Leukemia doesn’t form a lump like other cancers. It affects the blood, specifically the white blood cells, which normally help fight infection. In leukemia, these cells grow out of control and don't function properly. They can crowd out healthy blood cells, making it harder for the body to carry oxygen, fight infections, or stop bleeding.
There are different types of leukemia. Some grow slowly, like chronic lymphocytic leukemia or chronic myelogenous leukemia, and may not show symptoms for a long time. Others, such as acute lymphocytic leukemia or acute myelogenous leukemia, develop quickly and require immediate treatment.
Doctors usually find leukemia through blood tests or a bone marrow biopsy. But what leads someone to get tested? Is it persistent fatigue? Recurring fevers? Or perhaps a gut feeling that something just isn't right? Understanding how leukemia appears and how it's diagnosed can mean quicker action and better outcomes. So, how do we catch it early? What are the real signs we shouldn't ignore? And once it’s found—what can be done?
What Is Leukemia?
Leukemia is a cancer that begins in the blood and bone marrow. It mostly affects white blood cells, part of the immune system. These cells help the body fight infections. In leukemia, the body produces abnormal white blood cells that don’t work the way they should. These leukemia cells grow out of control and crowd out healthy blood cells, including red blood cells and platelets.
Imagine your bone marrow—the soft tissue inside your bones—as a factory that makes blood. It produces different types of blood cells: white cells (to fight infection), red cells (to carry oxygen), and platelets (to help stop bleeding). In leukemia, this factory gets flooded with defective white blood cells.
Over time, these abnormal cells take over the space, leaving little room for the normal blood cells the body needs. This is why people with leukemia often feel weak, bruise easily, or get infections more often.
How White Blood Cells Function—and What Goes Wrong in Leukemia
White blood cells protect the body from viruses, bacteria, and other threats. There are several kinds of white cells, each with a special job. For example, some directly attack germs, while others produce antibodies. When leukemia develops, the body starts making large numbers of immature or abnormal white blood cells that can't do their job properly.
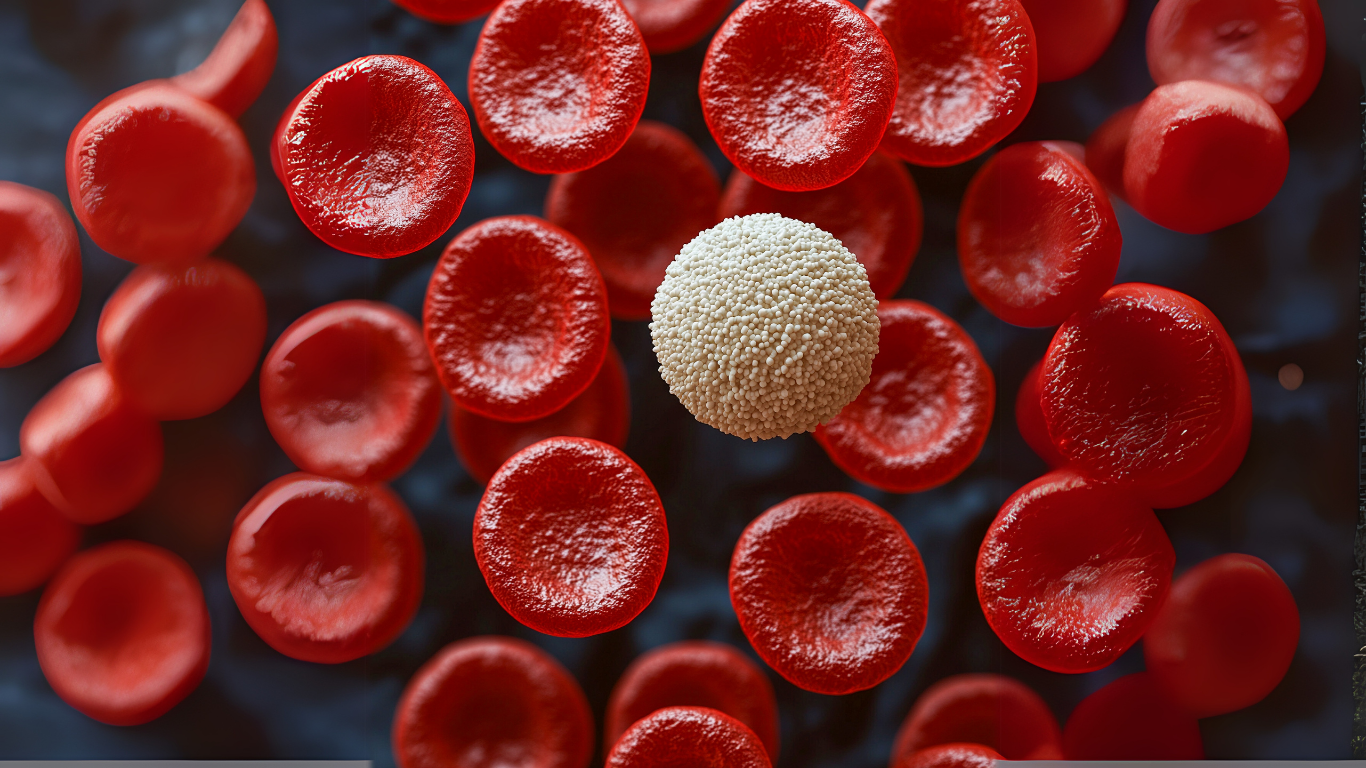
This not only weakens the immune system but also affects other blood cells. Red blood cells get reduced, leading to fatigue and shortness of breath. A shortage of platelets can cause easy bruising and bleeding. And because these leukemia cells don’t die when they should, they keep multiplying, making things worse over time.
Different Types of Leukemia
Leukemia isn’t just one disease. It comes in several forms. The most common are:
- Acute Lymphoblastic Leukemia (ALL)
This type of leukemia starts in early forms of lymphocytic white blood cells in the bone marrow. It's more common in children but can also occur in adults. It progresses quickly (hence the word “acute”) and requires urgent treatment.
A child with ALL might start feeling tired all the time, develop swollen lymph nodes, or bruise more easily than usual. In some cases, the leukemia can spread to the central nervous system, causing headaches or confusion.
- Acute Myeloid Leukemia (AML)
This form affects myeloid cells, which are responsible for producing red blood cells, some white blood cells, and platelets. AML can grow fast and is more common in adults, especially older adults.
A person with AML may visit a doctor after frequent nosebleeds, fevers, or a pale appearance. A complete blood count and bone marrow biopsy often reveal the cause.
- Chronic Lymphocytic Leukemia (CLL)
Unlike acute forms, chronic leukemia develops more slowly. Chronic lymphocytic leukemia affects immune cells called B lymphocytes. This type of leukemia is more common in older adults and might not show symptoms for years.
Some people are diagnosed with CLL after routine blood tests show an unusually high number of white cells. Over time, symptoms like swollen lymph nodes, fatigue, or frequent infections may appear.
- Chronic Myelogenous Leukemia (CML)
Chronic myelogenous leukemia begins in bone marrow cells that form blood. It can be silent in its early stages, with few symptoms. Later, it can behave more like an acute leukemia.
CML is linked to a genetic change called the Philadelphia chromosome, which causes bone marrow to produce leukemia cells uncontrollably.
Causes and Risk Factors of Leukemia
Leukemia doesn’t have one single cause. It develops when something changes the way bone marrow produces blood cells, especially white blood cells. In many cases, the exact reason is not clear.
However doctors and researchers have identified certain risk factors that seem to raise the chances of getting this disease. Some of these are genetic, while others are related to environment, lifestyle, or previous medical treatments. Understanding these factors can help people and doctors stay alert to possible early signs of leukemia.
Genetic Predisposition
Some people are born with a higher chance of developing leukemia because of changes in their genes. This doesn’t mean they will definitely get leukemia—but their risk is higher than average.
-
Family history: Having a close relative (like a parent or sibling) with leukemia can slightly increase the chance of developing the disease, especially chronic lymphocytic leukemia (CLL). This doesn’t guarantee anything, but it may lead doctors to monitor the person's blood cells more carefully over time.
-
Inherited genetic disorders: Conditions like Down syndrome, Li-Fraumeni syndrome, and Fanconi anemia are known to increase the risk of childhood leukemia, especially acute lymphoblastic leukemia (ALL) and acute myelogenous leukemia (AML). These conditions can affect how stem cells in the bone marrow grow and divide, which may lead to the production of abnormal blood cells.
-
Gene mutations in cells: Even people without inherited disorders may develop mutations in their bone marrow cells during their lifetime. These changes can turn healthy cells into leukemia cells, which grow out of control.
Environmental Exposures
Some outside factors have been linked to an increased risk of leukemia. These exposures may damage the DNA inside bone marrow cells, causing them to turn into cancer cells.
-
Radiation exposure: High levels of radiation—such as from atomic bomb exposure or certain radiation therapy treatments used in the past—can increase the chance of acute leukemia. This is especially true for acute myeloid leukemia (AML).
-
Chemical exposure: People who work with chemicals like benzene, which is found in oil refineries, chemical plants, or even cigarette smoke, may have a higher risk. Long-term exposure to such chemicals can damage stem cells and lead to abnormal white blood cells.
-
Previous cancer treatment: Some people who were treated for other cancers with chemotherapy or radiation therapy may later develop leukemia. These treatments, while aimed to kill cancer cells, can sometimes damage healthy blood cells in the bone marrow, especially in cases of acute myelogenous leukemia (AML).
Lifestyle and Other Contributing Factors
While lifestyle isn't always a direct cause of leukemia, certain habits or exposures can increase overall risk.
-
Smoking: Cigarettes contain harmful chemicals that are linked to many cancers, including leukemia. Smokers may have a higher chance of developing AML due to long-term chemical exposure.
-
Obesity: Being very overweight can affect the immune system and how the body handles cell growth. Some research suggests a link between obesity and acute leukemia, especially in children and young adults.
-
Age and gender: As shown in the table below, certain types of leukemia are more common in specific age groups and may be slightly more common in one gender.
-
Weakened immune system: People with immune suppression, whether from disease or medication (like after an organ or stem cell transplant), may face an increased risk of developing certain types of leukemia.
-
Long-term exposure to infections: Though not fully understood, some viruses have been studied for a possible link to leukemia development. This includes certain rare human viruses, but most common infections do not directly cause leukemia.
Common Symptoms of Leukemia
When something feels “off” in the body, it’s easy to assume it’s due to stress, lack of sleep, or a passing infection. But what if fatigue lingers for weeks? What if bruises appear without any injury? These could be signs that something deeper is going on—possibly in the blood and bone marrow.
Leukemia can start silently, affecting the production of white blood cells in the bone marrow, and slowly replacing healthy blood cells with abnormal cells. The symptoms may seem general at first—tiredness, fever, or frequent colds—but ignoring them may delay a leukemia diagnosis, especially in types like chronic leukemia, which progresses slowly.
General Signs and Symptoms of Leukemia
Many leukemia symptoms overlap with other illnesses, which can make them easy to dismiss. However, several common signs often appear when leukemia cells begin to interfere with the body’s normal processes:
-
Unexplained fatigue that doesn’t improve with rest
-
Frequent infections or illness due to weak immune system
-
Fever or chills, often without a clear cause
-
Bruising easily or bleeding that’s hard to stop
-
Pale skin (from low red blood cells)
-
Swollen lymph nodes, especially in the neck or underarms
-
Bone pain or discomfort, especially in long bones or joints
-
Loss of appetite or unexpected weight loss
-
Night sweats
People often say they “just don’t feel right” for weeks or months before seeking help. In some cases, leukemia is found during routine blood tests, even when no clear symptoms are present.
Differences in Symptoms by Leukemia Type
Each type of leukemia may show up in slightly different ways. Some forms progress quickly, while others develop over time, often without noticeable symptoms at first.
Acute Lymphocytic Leukemia (ALL)
This type usually affects children, but adults can get it too. Symptoms develop quickly, and the illness worsens fast.
-
Sudden fatigue and pale skin
-
Bleeding gums or nosebleeds
-
Bone or joint pain
-
Fevers with no clear cause
-
Difficulty breathing due to the buildup of leukemia cells
-
Swelling in the belly from enlarged liver or spleen
Acute Myeloid Leukemia (AML)
This type is more common in adults and also progresses rapidly.
-
Flu-like symptoms that don’t go away
-
Tiny red spots (petechiae) on the skin
-
Swollen gums or mouth sores
-
Bruising even with light pressure
-
Severe fatigue from low red blood cells
-
Recurring infections due to a weak immune system
Chronic Lymphocytic Leukemia (CLL)
CLL often affects older adults and may not cause symptoms early on. Many cases are found accidentally during routine blood tests.
-
Swollen lymph nodes without pain
-
Feeling full after eating only a little (from enlarged spleen)
-
Tiredness or weakness
-
Repeated respiratory infections
-
Weight loss over months
Chronic Myelogenous Leukemia (CML)
This type often has a slow, silent beginning and might not show symptoms for years.
-
Night sweats
-
Fullness or pressure in the upper abdomen
-
Tiredness that increases gradually
-
Pale skin
-
Fever, even when not sick
-
Easy bruising
When to See a Doctor
Sometimes the difference between a minor issue and something serious comes down to timing. If any of the symptoms listed above continue for more than a couple of weeks, or seem to be getting worse, it’s worth having them checked out.
Ask yourself:
-
Has this fatigue lasted longer than usual?
-
Are there bruises or bleeding that I can’t explain?
-
Have I been sick more often than usual?
If the answer is yes to any of these, your doctor may recommend:
-
A complete blood count (CBC)
-
Bone marrow biopsy
-
Blood or bone marrow tests to check for abnormal white blood cells
Catching leukemia early can improve treatment planning. Depending on the type of leukemia, treatment may include chemotherapy, targeted therapy, radiation therapy, or a bone marrow transplant or stem cell transplant.
The American Cancer Society and National Cancer Institute recommend not delaying testing if there are warning signs, especially for people with known risk factors, such as past radiation therapy, genetic conditions, or a family history of leukemia.
How Is Leukemia Diagnosed?
When people start feeling weak, bruise easily, or get sick more often than usual, they don’t always think it could be something like leukemia. However, the bone marrow could produce too many abnormal white blood cells behind these symptoms.
These leukemia cells multiply and push out healthy blood cells, which leads to problems like infections, fatigue, or bleeding. Since these signs can look like common illnesses, getting the right leukemia diagnosis early is important. Many people are diagnosed only after routine blood tests reveal unusual numbers. Others are diagnosed with vague complaints after repeated visits to doctors.
A correct diagnosis helps doctors determine a person's type of leukemia. It could be acute leukemia, which spreads fast, or chronic leukemia, which moves slowly. Each type may need a different kind of leukemia treatment, like chemotherapy, radiation therapy, stem cell transplant, or targeted therapy. Let’s look closely at the steps doctors follow to confirm a diagnosis and plan the next move.
Initial Evaluation and Medical History
When someone visits a doctor with symptoms like tiredness, fever, or swollen lymph nodes, the doctor will first ask detailed questions. These may include:
-
How long have the symptoms been going on?
-
Are there any infections that won’t go away?
-
Any unusual bleeding or bruising?
-
Has there been unexplained weight loss?
-
Do you have a family history of blood disorders or cancer diagnosis?
The doctor may also ask about past radiation therapy, exposure to chemicals, or whether the patient has other risk factors that raise the chance of leukemia. A physical exam may show swollen lymph nodes, an enlarged spleen or liver, or signs of bleeding.
This conversation is critical. Sometimes, the full picture only becomes clear after the doctor pieces together symptoms and test results.
Complete Blood Count (CBC)
A complete blood count (CBC) is often the first test done. It measures the number of red blood cells, white blood cells, and platelets in the blood. In leukemia, these counts are often abnormal.
What doctors look for:
-
Too many or too few white blood cells
-
Low red blood cell count (anemia)
-
Low platelet count (risk of bleeding)
In some cases, leukemia cells can be seen directly in the bloodstream. If the CBC is unusual, more tests follow.
Peripheral Blood Smear
After a CBC, the doctor may request a blood smear, where a drop of blood is examined under a microscope.
This helps identify:
-
Abnormal white blood cells
-
Immature blood cells that shouldn’t be in the bloodstream
-
Clues about whether it’s a lymphocytic leukemia or myeloid leukemia
Seeing these abnormalities gives doctors a clearer idea about the need for further testing.
Bone Marrow Biopsy and Aspiration
This test is one of the most accurate ways to confirm leukemia. It involves removing a small amount of liquid bone marrow (aspiration) and a small core of solid bone marrow tissue (biopsy), usually from the hip bone.
It helps doctors see:
-
The number and type of leukemia cells
-
How crowded the bone marrow is
-
How many healthy blood cells are still being made
The sample is sent to a lab, where experts look at the cells and identify which type of leukemia it is—acute lymphocytic leukemia, acute myeloid leukemia, chronic lymphocytic leukemia, or chronic myelogenous leukemia.
Immunophenotyping
This test checks for specific markers on the surface of cells using a method called flow cytometry. It helps doctors figure out which kind of white blood cells have turned into leukemia cells.
This is important because different lymphocytic or myeloid leukemia types need different treatments. For example, chronic lymphocytic leukemia (CLL) is treated differently from acute myelogenous leukemia (AML).
Cytogenetic and Molecular Tests
Sometimes, cancer cells carry changes in their chromosomes or genes. These changes help confirm the leukemia diagnosis and also help doctors predict how the disease may behave.
Tests used:
-
Cytogenetics: Looks for extra, missing, or changed chromosomes
-
FISH (Fluorescence In Situ Hybridization): Finds specific genetic changes
-
PCR (Polymerase Chain Reaction): Detects very small changes in DNA
For example, chronic myelogenous leukemia (CML) is almost always linked to the Philadelphia chromosome, a change in DNA that can be detected with these tests.
Imaging Tests
Though leukemia usually doesn’t form solid tumors, imaging can help doctors check if the disease has affected the lymph nodes, spleen, liver, or central nervous system.
Tests may include:
-
Ultrasound: To check spleen or liver size
-
CT scan: To detect enlarged organs or lymph nodes
-
MRI or spinal tap: If there are signs the central nervous system may be affected
These tests are especially helpful in advanced leukemia or when symptoms like headaches or vision changes appear.
Lumbar Puncture (Spinal Tap)
In cases where leukemia may have spread to the central nervous system, a lumbar puncture is done to check for leukemia cells in the spinal fluid.
This is more common in:
-
Childhood acute leukemia
-
Adults with acute lymphocytic leukemia
-
Leukemia cases where the patient has neurological symptoms
Finding cells here can change the leukemia treatment plan, including the need for chemotherapy delivered into the spinal fluid.
Importance of Early and Accurate Diagnosis
Early diagnosis can give patients a wider range of treatment choices. In acute leukemia, treatment usually starts right after diagnosis because the disease progresses quickly. In chronic leukemia, treatment may not begin immediately, but careful monitoring is still needed.
A late diagnosis can lead to:
-
More damage to bone marrow
-
Lower healthy blood cell counts
-
Greater spread of leukemia cells to other organs
-
Limited response to treatment
Accurate tests also help decide if newer treatments, such as targeted therapy, clinical trials, or stem cell transplantation, are options.
Leukemia Treatment Options
When someone is diagnosed with leukemia, it can feel overwhelming. There's the word "cancer" and then a long list of tests, medical terms, and treatment plans that follow. But the goal of treatment is not always the same for every patient.
For one person, the aim might be to kill leukemia cells and achieve long-term remission. For another, the goal may be to manage the condition if it’s slow-growing, like in chronic leukemia. Treatment choices depend on many things: the type of leukemia, age, general health, genetic changes in the leukemia cells, and how far the disease has progressed in the blood and bone marrow.
Some treatments aim to completely wipe out abnormal white blood cells, while others focus on helping the body produce more healthy blood cells. Options can range from powerful drugs to stem cell transplants and newer therapies like immunotherapy.
In certain cases, patients may even join clinical trials to try treatments that are still being tested but have shown hope. The first step in choosing the right path is always a clear diagnosis, often confirmed by blood tests, a bone marrow biopsy, and sometimes genetic testing.
Understanding the Treatment Approach
The main goals of leukemia treatment are:
-
Stop the growth of leukemia cells
-
Allow the bone marrow to make normal blood cells again
-
Prevent the spread to organs like the central nervous system
-
Reduce the chance of relapse
Doctors consider:
-
Whether the leukemia is acute or chronic
-
If it affects lymphocytic or myeloid cells
-
Age and existing health issues
-
Specific genetic changes (like the Philadelphia chromosome in chronic myelogenous leukemia)
For acute leukemia, treatment usually begins immediately. With chronic leukemia, like chronic lymphocytic leukemia (CLL) or chronic myelogenous leukemia (CML), some patients may be monitored for a while before starting therapy.
Chemotherapy
Chemotherapy uses strong drugs to kill cancer cells or stop them from growing. It's often the first treatment for acute lymphocytic leukemia, acute myeloid leukemia, and some childhood leukemia cases.
Treatment involves:
-
Intravenous (IV) or oral drugs, sometimes both
-
Several cycles over weeks or months
-
Supportive care to manage side effects
Common side effects:
-
Hair loss
-
Low red blood cells (anemia)
-
Increased risk of infection due to low white blood cells
-
Nausea or mouth sores
Although side effects can be tough, chemotherapy is often effective at pushing leukemia into remission.
Radiation Therapy
Radiation therapy uses high-energy rays to kill or slow the growth of leukemia cells. It's not the main treatment for all types but can be useful in certain situations.
Doctors may use it to:
-
Treat leukemia that has spread to the brain or spinal cord
-
Shrink swollen lymph nodes or enlarged spleen
-
Prepare for a stem cell transplant
A person with acute leukemia who develops headaches or neurological symptoms might get radiation to the brain to stop the spread into the central nervous system.
Targeted Therapy
Targeted therapy attacks specific molecules or genetic changes found in leukemia cells. Unlike chemotherapy, which affects both healthy blood cells and cancerous ones, targeted drugs are more precise.
Examples:
-
Imatinib for chronic myelogenous leukemia (CML) with the Philadelphia chromosome
-
Venetoclax for certain forms of chronic lymphocytic leukemia (CLL)
These drugs are usually taken as pills and often have fewer side effects than chemotherapy.
Immunotherapy
Immunotherapy uses the body’s immune system to fight leukemia cells. This may involve:
-
Monoclonal antibodies that attach to leukemia cells and mark them for destruction
-
CAR T-cell therapy, where a patient’s own immune cells are changed in a lab to recognize and attack cancer cells
This is a newer option and is often used when other treatments haven’t worked, especially in relapsed leukemia.
Stem Cell Transplant
A stem cell transplant replaces damaged or cancerous bone marrow with healthy stem cells, either from the patient or a donor. It's also called a bone marrow transplant.
Steps:
-
High-dose chemotherapy or radiation therapy to destroy existing marrow
-
Infusion of stem cells through a vein
-
Recovery while the new marrow cells begin to grow
This is often recommended for patients with high-risk types like acute myelogenous leukemia (AML) or for those who relapse.
Clinical Trials and Emerging Treatments
Some patients join clinical trials to access new or experimental therapies. These trials are monitored closely and often supported by institutions like the National Cancer Institute or American Cancer Society.
Types of emerging treatment:
-
New targeted therapies
-
Second-generation CAR-T cells
-
Drugs that affect leukemia cell metabolism or gene expression
A patient who hasn’t responded to regular leukemia treatment may be eligible to join a trial, giving them another chance when standard therapy is no longer enough.
Treatment for Chronic Leukemia
Chronic leukemia, such as chronic lymphocytic leukemia (CLL) and chronic myelogenous leukemia (CML), may not need treatment right away.
Instead, doctors may recommend:
-
Watchful waiting: regular check-ups to monitor blood cells
-
Starting treatment if symptoms develop or leukemia cells multiply quickly
For CML, targeted therapy with tyrosine kinase inhibitors (TKIs) often keeps the disease under control for years.
Supportive Care During Treatment
Leukemia treatment affects more than just the cancer. It can weaken the body in many ways. Supportive care focuses on:
Treating infections
Managing anemia with red blood cell transfusions
Preventing bleeding with platelet transfusions
Using growth factors to boost white blood cells
This helps patients stay strong enough to complete their treatment and recover safely.
Emotional and Practical Support
Living with leukemia is more than just following a treatment plan. Many patients feel overwhelmed, especially during long hospital stays or after hearing difficult news. Support includes:
-
Counseling or support groups
-
Talking to others with similar diagnoses
-
Help managing work, childcare, or financial planning
Families are often part of the journey, especially in childhood leukemia or when someone needs a stem cell transplant from a sibling or relative.
Living With Leukemia
Being diagnosed with leukemia changes how someone looks at everyday life. Some people need to start treatment right away, especially those with acute leukemia, while others with chronic leukemia may live with the disease for years before starting any therapy.
No matter the type of leukemia—whether it’s chronic lymphocytic leukemia, acute lymphocytic leukemia, or acute myelogenous leukemia—the journey doesn't end at diagnosis. There are ups and downs: some days feel normal, and others are filled with hospital visits, tests, or side effects.
How someone manages daily life depends on the kind of treatment they are getting, how their body is responding, and the support they have. Simple things like keeping track of medications, understanding how leukemia cells affect healthy blood cells, or knowing when to seek help make a big difference.
Managing Fatigue and Everyday Energy
Fatigue is one of the most common and long-lasting effects of leukemia and its treatment. It can affect both physical strength and mental focus. For someone getting chemotherapy, radiation therapy, or recovering from a bone marrow transplant, this tiredness can feel like walking through quicksand.
Ways to manage:
-
Plan the day with rest breaks
-
Ask for help with chores or errands
-
Use a journal to track when energy levels are higher
-
Eat meals that support red blood cells, like iron-rich foods
A person with chronic myelogenous leukemia on targeted therapy may still feel this kind of tiredness, even if their blood tests are stable.
Coping With Infections and a Weak Immune System
Since white blood cells are responsible for fighting infection, anyone with leukemia—especially during treatment—faces an increased risk of getting sick. This can happen even from mild colds, cuts, or stomach bugs.
Steps to lower the risk:
-
Wash hands often and avoid crowded places
-
Stay away from people with flu or infections
-
Keep surfaces clean at home
-
Follow the doctor’s advice on vaccinations
If a person develops a fever during a stem cell transplant or after chemotherapy, it can be a medical emergency. Many patients carry a thermometer and are told to report temperatures over 100.4°F (38°C) immediately.
Keeping Up With Emotional and Mental Health
Getting a cancer diagnosis changes how people think about their future. Fear, sadness, and stress are normal reactions. For some, these feelings become overwhelming, especially during intense treatments like a bone marrow biopsy or stem cell transplantation.
Helpful steps:
-
Talk openly with trusted friends or family
-
Join support groups (online or in person)
-
Ask for a referral to a counselor or psychologist
-
Explore relaxation techniques like breathing exercises or journaling
People with chronic lymphocytic leukemia (CLL) who are told they can "wait and watch" may still feel anxious even without current symptoms.
Returning to Work, School, or Routine
Getting back to normal routines after leukemia treatment isn't always easy. Some people feel ready after a few weeks; others take longer due to lasting fatigue, blood cell recovery, or emotional healing. Children with childhood leukemia may return to school part-time while still on treatment.
Tips for a smoother transition:
-
Talk with employers or schools about needed adjustments
-
Be open about energy levels and limits
-
Start with reduced hours or partial days
-
Follow up on all recommended tests to track progress
Many adults with chronic leukemia continue working during oral treatments but may need flexibility for frequent lab visits or side effect management.
Staying on Top of Long-Term Monitoring
Even after treatment ends, regular monitoring is key. Leukemia cells can return months or years later. Doctors use blood tests, bone marrow biopsies, and sometimes genetic testing to track recovery and detect any signs of relapse.
Important follow-up tasks:
-
Keep appointments for labs or scans
-
Watch for signs like new bruising, fever, or swollen lymph nodes
-
Ask about potential late side effects of treatment (like heart issues or hormone changes)
-
Know when to contact the care team between visits
Someone treated for acute myeloid leukemia with a stem cell transplant may need check-ups for years to come. Long-term survivors are often monitored closely by both oncologists and primary care doctors.
Conclusion
At PHO, we understand that facing leukemia—whether it’s acute leukemia, chronic lymphocytic leukemia, or chronic myelogenous leukemia—can be one of the most difficult experiences for a child or young adult and their family. That’s why our focus goes beyond just treating the disease. We provide holistic care across every stage—from early signs, leukemia diagnosis, and individualized treatment plans, to ongoing support during recovery and long-term follow-up.
Our experienced team of doctors, nurses, and support staff specializes in treating blood and bone marrow disorders, with a deep understanding of how leukemia cells affect growing bodies. We use the latest tools for blood tests, genetic testing, bone marrow biopsy, and modern therapies like targeted therapy, immunotherapy, stem cell transplant, and participation in clinical trials.
We are committed to providing care that’s not only medically advanced but also emotionally supportive. Every child is different, and our team tailors care to meet individual needs—supporting families every step of the way, from diagnosis to full recovery.
PHO Offers Comprehensive Care in the Treatment of:
-
Leukemia (ALL, AML, CLL, CML)
-
Lymphomas (Hodgkin and Non-Hodgkin)
-
Bone marrow failure syndromes
-
Platelet and clotting disorders
-
Anemia and other red blood cell conditions
-
Immune system disorders
-
Preparation and care for bone marrow transplant or stem cell transplant
FAQs
-
Can leukemia be cured? Yes, many children and young adults are cured of leukemia, especially when diagnosed early and treated appropriately.
-
Is chemotherapy always needed for leukemia? Not always. Some types, like chronic lymphocytic leukemia, may not need immediate treatment. Your doctor will decide based on the type and stage.
-
How often will my child need follow-up care? Follow-up schedules vary but typically include regular blood tests and physical exams for several years after treatment.
-
Are there any long-term effects of leukemia treatment? Some treatments may affect growth, fertility, or organ function, which is why long-term monitoring is important.
-
Can my child go to school during treatment? Many children return to school during or after treatment with support from their care team and school staff.







Comments